How Sex Can Change During (Peri)Menopause
by Stephanie AuteriShare
I don’t know if they’ve always been there, floating about in the ether, and I’m just now noticing them because of my age/circumstances or if their proliferation is an indication that we’re finally having much-needed conversations about female sexuality and reproductive health, but there have been a lot of new books on perimenopause/menopause.
Last year, MK Czerwiec came out with Menopause: A Comic Treatment, a graphic anthology. The other month, I received a copy of Maisie Hill’s Perimenopause Power. And I am for sure looking forward to Jennifer Gunter’s The Menopause Manifesto and Heather Corinna’s What Fresh Hell Is This?.
I’m only 40, but I’m already starting to see the signs. Poor sleep. Night sweats. Fatigue. Brain fog. More frequent migraines. More bloating. Bladder issues. Dry mouth.
Last month, I was feeling especially murder-y and then I read in Hill’s book that perimenopause could be marked by, “ALL THE RAGE, ALL THE TIME.”
Exasperated, I tweeted, “Is it perimenopause, the pandemic, or my usual personality?”
Anyway. Our bladders and brains aren’t the only things impacted by perimenopause and menopause. Our sexuality changes as we age, too.
What’s the Difference Between Perimenopause and Menopause?
Before we get into it, let’s define perimenopause and lay out how it differs from menopause. After all, though menopause has been the punchline of many jokes about aging for a good long while, the use of the term “perimenopause” in public conversation is still fairly new.
So, here’s the lowdown. While menopause typically happens between the ages of 45 and 55, perimenopause can begin anywhere from four to 15 years before then. Hill writes that it’s often marked by a shortened menstrual cycle, along with a varying cycle length and fluctuating hormone levels. You may find yourself experiencing “menopausal” symptoms.
As for menopause, it’s not that long stretch of unbearable hot flashes we’ve been imagining. Rather, it’s a single day: the one-year anniversary since your last menstrual period.
The years after that, when your periods are kaput and those hot flashes and other symptoms increase, are actually called postmenopause.
As for what’s going on inside your body, that information could fill an entire book (or four). If you’re interested in those basics, I recommend checking out the resource pages put together by the Office on Women’s Health.
What About My Sex Life?
Now that that’s out of the way, let’s get down to business. As you move into your late 30s and early 40s, you may notice several shifts in your sex life as your estrogen levels drop.
For one, you’ll likely experience some degree of vaginal atrophy. This means the walls of your vagina will become thinner and less elastic. You’ll also experience a reduction in your normal vaginal secretions, which can lead to dryness. These changes can cause itching, burning, pain, and other discomfort, which, in turn, can lead to pain during penetrative intercourse. Doesn’t sound like fun, right?
At this point, some people turn to hormone therapy to give their estrogen levels a bump. But this option isn’t right for everyone and may, in fact, carry a variety of health risks depending upon your medical history. If you’re curious about hormone therapy, I recommend talking to your OBGYN about the various options out there and the research that exists around side effects and impact on menopausal symptoms.
Hormone therapy aside, there are other options. If you want to make penetrative sex less painful, you can buy an over-the-counter vaginal moisturizer or personal lubricant (and, hell, I recommend this for people of any age).
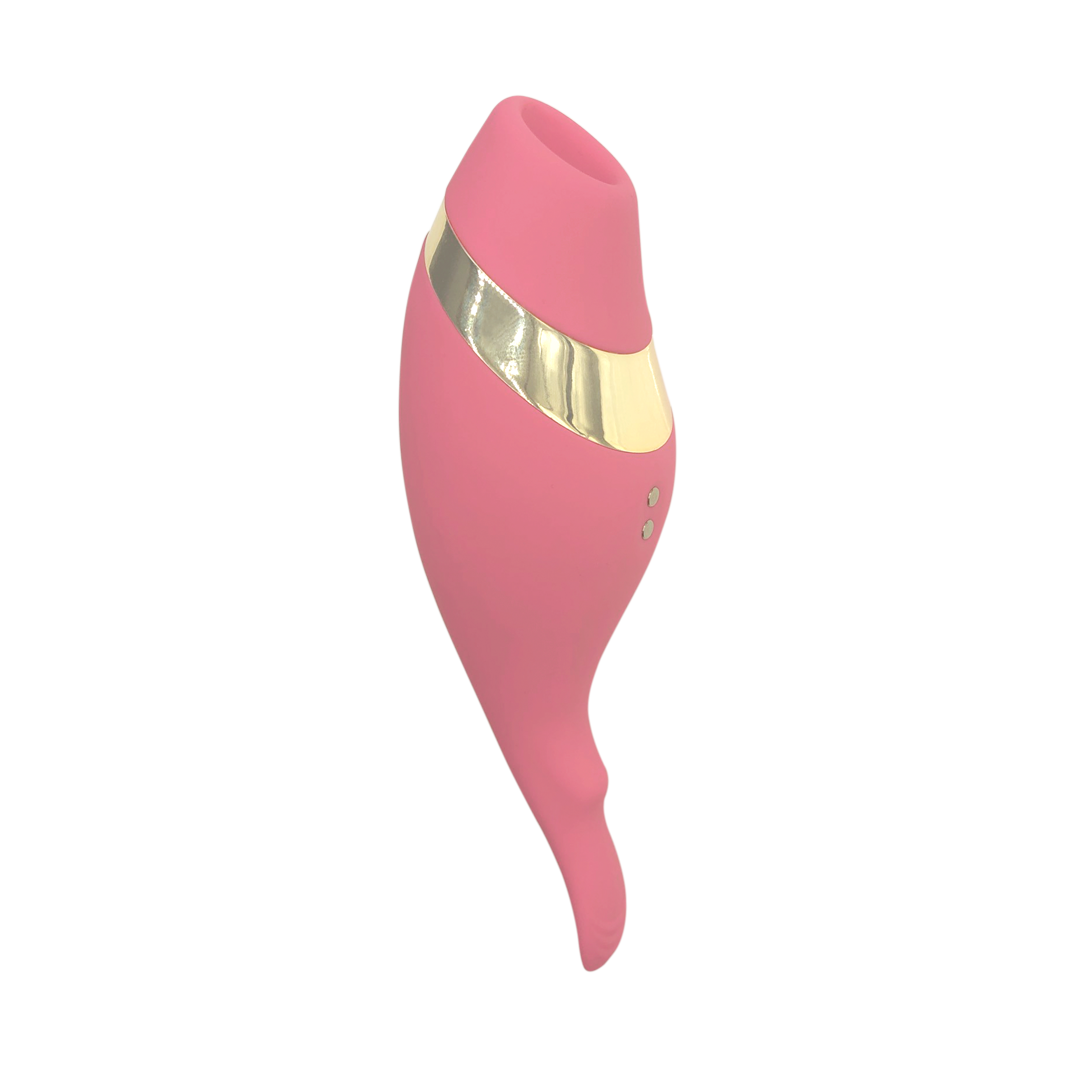
If you want to engage in vaginal exercise, you can play around with vaginal dilators and other toys, which can help to maintain the elasticity of your vaginal walls. Or you can be more intentional about having penetrative sex more frequently.
Your doctor may also prescribe a hormonal contraceptive, or an estrogen cream, gel, or ring.
Personally, I think the best thing to do when penetrative sex is painful is to expand the definition of what sex means to you. Penetrative sex doesn’t have to be the main event. I’ve written about this at length before but, when you give yourself the chance to enjoy all the other forms of pleasure that exist, you may find that your sex life undergoes a revitalization of sorts. A sexual relationship that revolves around penetrative sex is very limiting.
Once you’ve dealt with your vaginal atrophy, you may also notice that your levels of sexual desire have shifted.
In some cases, those going through (peri)menopause experience an increase in sexual desire. This is often due to lifestyle factors, such as kids leaving the nest, allowing you more alone time and quality couple time. In the case of postmenopause, the increase could be due to the elimination of anxiety over the possibility of an unplanned pregnancy. Some women just plain feel more comfortable in their sexuality by that point in their lives.
In other cases, those going through (peri)menopause may feel less desire and arousal. They may experience depression and anxiety around the changes in their body, lack of sleep thanks to other menopausal symptoms, and sometimes, it’s just lower levels of estrogen that lead to a decreased sex drive and the fact that it takes longer to get aroused.
In these cases, it’s worth talking to your OBGYN so that you can find a treatment that tackles the underlying cause of your diminishing interest in sex.
Continue to Communicate with Your Partner
No matter how the symptoms of (peri)menopause manifest in your body, it’s important that you communicate with your partner(s) about what you’re experiencing. Chances are, they’ve noticed a shift in your sex life too, but have no clue what’s causing it.
Finally, remember that perimenopause, menopause, and postmenopause are not problems to be fixed. They’re just natural aspects of growing older.
As long as you keep this front of mind, you’ll be able to roll with anything.


 Give in to the Kinky Countdown
Give in to the Kinky Countdown
 Quiz: Gifts For Your Love Language
Quiz: Gifts For Your Love Language
 Five Aphrodisiac Foods For Valentine’s Day
Five Aphrodisiac Foods For Valentine’s Day